Introduction to this Blog Series
This blog will serve as the first part in a multi-part blog series addressing new technologies attempting to improve your knee replacement outcomes. This series will present advancements discussed in the scientific literature in an easy to understand manner for you to have well informed discussions with your healthcare team before your knee replacement. Please keep in mind that not all of the technologies discussed in this blog series will be available to everyone. This first part will discuss patient specific instrumentation (PSI).
What is Patient Specific Instrumentation
The success of your knee replacement largely depends on the proper alignment of the knee implant with the bones that surround your knee as well as the space that makes up the knee joint. [1] Patient specific instrumentation (PSI) is a novel system that uses 3D imaging and 3D printing to theoretically improve knee replacement surgeries. [1] The main components of PSI are:
1)3D imaging - either computed tomography (CT) or magnetic resonance imaging (MRI)
2)3D printing of customized cutting blocks
Before the knee replacement, a 3D image of your knee will be taken using either a computed tomography (CT) scan or magnetic resonance imaging (MRI). This image will allow your surgeon to design a surgical approach tailored to your knee. 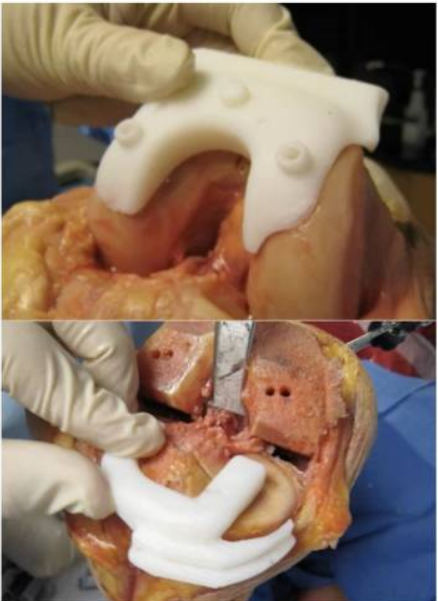
Following this personalized plan, customized cutting blocks will be rendered using 3D printing. An example cutting block is shown in the image above. These customized cutting blocks theoretically allow more accurate cutting and placing during your procedure by acting as a guiding stencil for your surgeon.
What does the evidence say about Patient Specific Instrumentation?
There is currently no consensus on whether it is a better or worse approach than traditional knee replacement surgery.
Some studies with a small number of patients suggest that this is a better approach to knee replacement surgeries. One study showed that PSI slightly reduced surgical time. [2] The study authors compared 57 knee replacements done using the PSI approach to 57 knee replacements done using the traditional approach. All 114 surgeries were done by the same surgeon. The results showed that the PSI approach reduced surgical times by 12.1 minutes. This is relevant as knee replacements take on average between 1-3 hours, [3] which means in the time a surgeon can perform 5 knee replacements using the traditional technique, 6 knee replacements can be done using the PSI method. Another study showed that PSI leads to greater improvement in function. [4] The study authors compared 42 knee surgeries done using the PSI approach to 40 knee surgeries done through the traditional method. All surgeries were done by the same surgeon. Function was measured 6-months after the completion of the surgery by scoring people on their ability to go from sitting to standing, walking and moving independently. The PSI approach led to a 24.5 point improvement in function score, while the traditional approach led to a 3.8 point improvement in function score.[4]
On the contrary, other studies have shown that this approach is no better than the traditional approach to knee replacement surgeries. One study showed that PSI did not lead to improved limb alignment during surgery. [5] The study authors conducted a systematic review and included 22 articles in their study. This is important as systematic reviews are a type of study design that requires the authors to thoroughly review all of the relevant studies on this topic and present a much stronger level of evidence than any single research study.
There is no accurate and complete analysis comparing the costs of the two approaches in the resesarch literature.[1] However, cost should be an important consideration in future research.
Conclusion
Patient specific instrumentation is just one of the many advancements that continue to be made to improve knee replacement surgeries. PSI is an approach characterized by imaging your knee before surgery, to allow your surgeon to design a surgical approach tailored to your knee, and rendering tailored cutting blocks. Although potentially promising, there is currently no consensus on whether PSI is better than the traditional knee replacement procedure.
Do you need an app to help you with your daily recovery after your knee replacements? In need of an effective guide to your recovery? Try the Curovate app,
an evidence-based physcial therapy app
that will provide you with a physical therapy plan, guided video exercises and
video physical therapy to assist you along your journey to recovery! Download Curovate today by clicking the links below!









