Woman jogging. How can I prevent an ACL tear? Image by roxanawilliams1920 from Pixabay.com.
The Anterior Cruciate Ligament (ACL) is a knee ligament that connects the lower leg (tibia) to the thigh (femur). The role of the ACL is to prevent the tibia from moving forwards relative to the femur and it provides stability to the knee during movement. The ACL is a commonly injured ligament, often requiring surgery and a long recovery process, with significant loss of function and mental stress during the recovery. In the United States, it is estimated that at least 200,000 people tear their ACL every year. [11]
Approximately 75% of ACL injuries are non-contact, meaning they were not the result of another person applying a direct force on the injured person’s knee. [11] The typical way to injure your ACL is a change in direction or speed (acceleration and deceleration), or landing from a jump, which results in the knee caving inwards or hyper-extending. [6][11] These movements cause the lower leg to move forward relative to the thigh, which places substantial stress on the ACL.
To prevent ACL injuries you must consider risk factors and how to address them. There are two main categories of risk factors, known as extrinsic and intrinsic. Intrinsic risk factors are related to the person at risk, for example if they have weak muscles on the side of their hips (abductors), they may be more likely to allow their knee to cave in during activity which can lead to an ACL injury. [8] Extrinsic risk factors are ones that are beyond the traits of the person at risk, so for example playing on artificial turf leads to more ACL injuries than grass.[4] Within both of these categories there are modifiable risk factors that can be changed and non-modifiable risk factors that can not be changed. The main focus of this blog is on intrinsic, modifiable risk factors because these are things about you that you can change to decrease your risk of tearing your ACL.
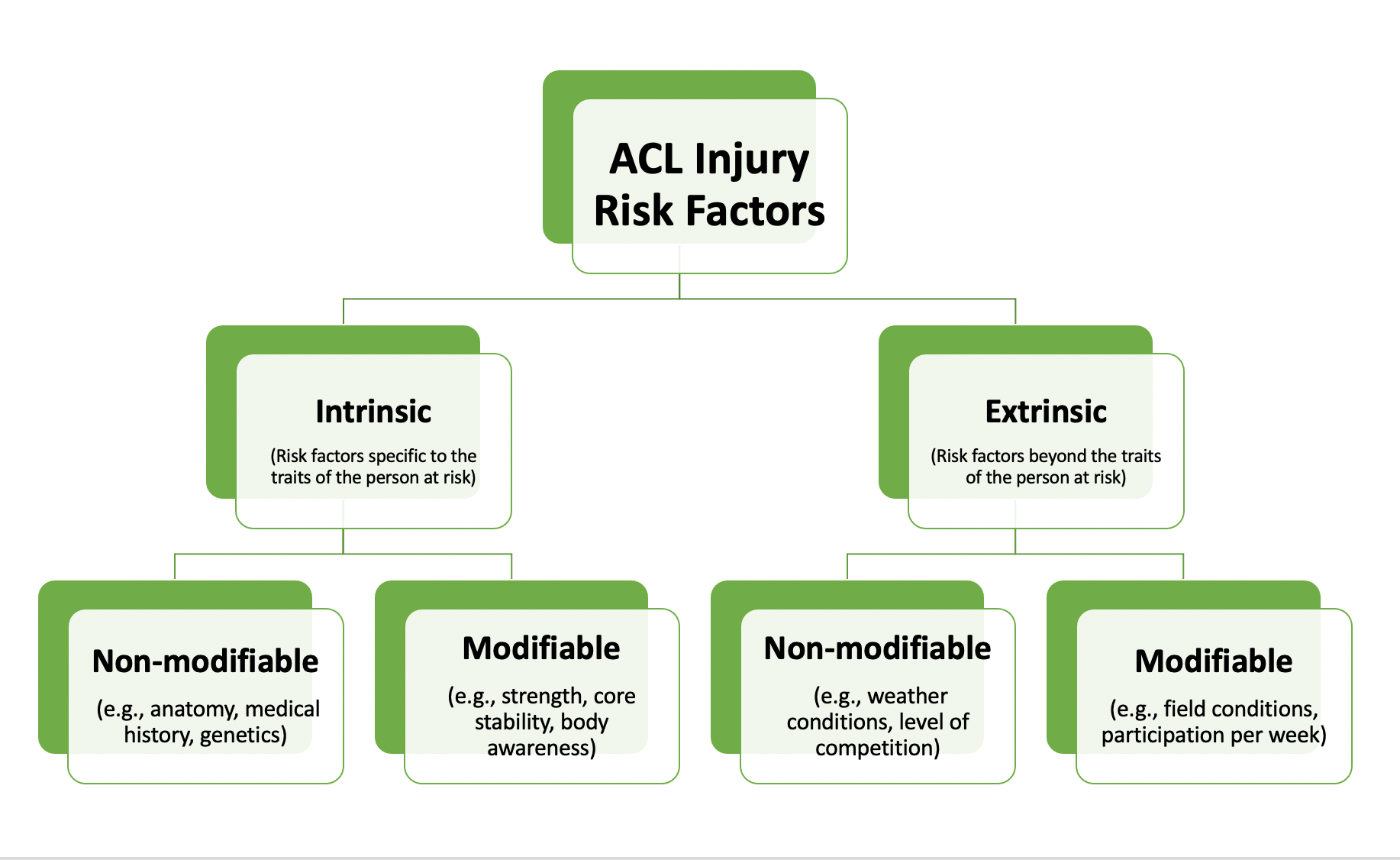
What are the extrinsic modifiable and non-modifiable risk factors?
Extrinsic risk factors have to do with the playing environment, weather conditions, equipment, and level of play. Some examples of these include increased risk of an ACL tear when playing on artificial turf [4] or when the conditions are dry and there has been limited rainfall for field sports. [8] In skiing, icy or snowy conditions lead to a higher rate of ACL injury. [8] ACL injuries are also more common in college-level athletes than high-school athletes and are more likely to occur with sport participation of greater than 4 times per week. [8] In American college teams, the highest rates of ACL injuries were in football for men, and basketball, soccer and field lacrosse for women. [7][8] It is important to note that some of these factors are modifiable and can be changed by you as a participant, like what sport you compete in, as well as how often and at what level you compete at. However, there are other ways to prevent injury that don’t involve stopping competition in a sport you enjoy, which will be explained below.
What are the intrinsic risk factors that I can’t change?
Intrinsic non-modifiable risk factors have to do with a person’s medical history, anatomy, and genetics; things about yourself that you can’t change. Previous injury either to the same ACL, the other ACL, or to the same side ankle ligaments increase ACL injury risk. [8][9] A person’s anatomy plays a factor, as having a looser knee (known as increased laxity) and having knees that have excessive hyper-extension (called genu recurvatum) increases risk of ACL injury. [1][8][9] Other anatomical features like the shape of the tibia and femur and decreased length, width and volume of the ACL also increase the risk of a tear. [1][8] Individuals with a difference in the length of their legs are also at a higher risk of injury, typically in the shorter leg. [9]
There are also significant genetic factors and family history that influence injury risk as well. [8][9] Sex is a notable genetic factor as females are at a higher risk of ACL tears.[9]There are a number or anatomical factors that influence the way women move and the loads placed on the ACL that contribute to this increased risk. These are things about you that can’t be changed; however, the impact they have on your movement are things that can be accounted for to some degree, which leads to the intrinsic modifiable risk factors.
What are the intrinsic risk factors that I can change?
The intrinsic modifiable risk factors have to do with how your body moves, which is referred to as your biomechanics. Neuromuscular control has to do with how your brain and nervous system activates your muscles, which as a result controls your biomechanics. Appropriate activation and strength of the key muscles in the leg is critical to controlling movement and preventing undue stress on the ACL.
As mentioned before, the collapse of the knee inwards, hyper-extension of the knee, and a reduction in knee flexion during changes in direction, stopping abruptly or landing from a jump are the main mechanisms of injury for the ACL. These movements are partially a result of a person's anatomy, for example females tend to have a wider pelvis which leads to a larger angle at the knee, called the Quadriceps (Q) angle (see image below). This increased angle leads to a greater chance of the knee collapsing inwards, tearing the ACL. Where neuromuscular control comes in is that the muscles that resist that movement are weak, there is a greater chance of injury. In this case it is weak hip abductors and external rotators that increase the risk of an ACL tear due to their inability to resist the collapse of the knee. [8][9]
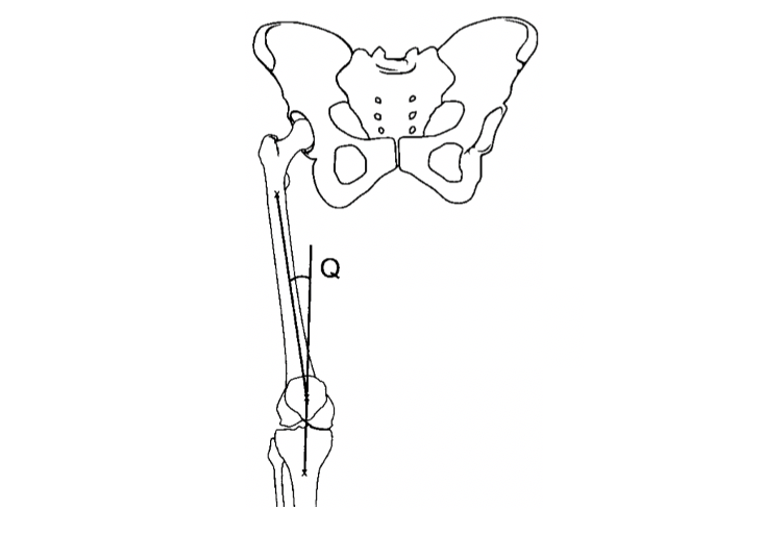
Image from Sanfridsson et al. (2009). [10]
The same is true with weak hamstrings which are the large muscles on the back of the thigh that also contribute to the control of the knee joint. If these muscles are weak, or at least if they are significantly weaker than the large quadricep muscles on the front of the leg, there is an increased risk of ACL tear.
Core stability and strength of the core muscles in the lower back and abdominal area are also important. Having poor core strength and stability increases injury risk.[8][9] Improving core stability can help to promote good movement patterns that don’t put excessive stress on the ACL. The same is true with proprioception, which is the ability to sense where your body is in space. If you have poor proprioception, you lack body awareness which can lead to you inadvertently putting yourself in positions that stress the ACL and this increases your risk of a tear.[3][8][9]
Another factor that influences how your body moves is your body weight and the ratio of your body weight to your body height; which is called your body mass index (BMI). People with a higher BMI are more likely to tear their ACL due to the extra load on the knee and the influence this has on a person's movement patterns.[5]
So are you at risk of tearing your ACL?
Your risk depends on many different factors listed above, as well as how they interact with each other. Although there are some risk factors you may have that you can’t change, don’t let this stress you out or prevent you from participating in the activities you enjoy. Focus on the things you can change!

Image by Renno_new from pixabay.com
How can I prevent an ACL tear?
Regardless of how many of the risk factors above that you have, there are still things you can do to prevent an ACL tear. These primarily have to do with improving the strength of your hip abductors, hip external rotators, and hamstring muscles, as well as improving your core stability and body awareness (proprioception) as deficiencies in these areas increase your risk of injury.[2][9]
A review of a number of different injury prevention programs suggested the following activities for ACL injury prevention. Strengthening programs (especially for athletes at lower levels of competitions), core stability training, speed and power training (plyometrics) with a focus on quick change in direction and jumping, and balance training.[2][3] Feedback about your movement patterns should also be provided during all components of a training program to encourage development of body awareness and good movement patterns.[3] Providing education on proper movement patterns, specifically landing technique is also recommended.[3] These strategies will help to develop your physical literacy, which is your confidence and competence in movement, something that is helpful for preventing injuries in general.
Conclusion
ACL tears happen relatively frequently in sport and physical activity of all levels. There are a number of different factors that may contribute to your risk of injury, many of which you can’t control. By focusing on the factors you can control such as improving the strength of your hip abductors, hip external rotators, and hamstring muscles, as well as improving your core stability and proprioception, you can help to reduce your risk.
The Curovate mobile app has nonoperative and operative ACL injury rehabilitation programs developed by a Physical Therapist to help you improve function and strength after an ACL injury. Curovate is a great tool to get you back to the activities you enjoy after injury and help you prevent future ACL injuries. To download the app, check out the links below.
If you need further customized assistance during your surgery or injury recovery check out our Virtual Physical Therapy page to book your 1-on-1 video session with a physical therapist.
 |
 |
|---|
Other Blogs Related to ACL Injury
- What is an ACL and How is It Injured?
- I injured my ACL, what should I do?
- Why female soccer players suffer more ACL injuries
- Turf leads to more ACL injuries - fact or fiction?
- How to prevent ACL injuries
- When can I return to sport after an ACL injury or surgery?
- After I wake up from ACL surgery, what should I expect?
- What does my ACL recovery timeline look like?
- Is ACL surgery painful?
- Where is my new ACL coming from? What are the most common areas for an ACL graft?
- Can an ACL injury lead to arthritis in the future?
- Did I retear my ACL graft?
- Is my ACL graft weaker than my original ACL? Or is my ACL graft stronger than my original ACL?







