Image by Fly View Productions via Canva
Knee replacement surgery is one of the most commonly done and cost-effective musculoskeletal surgical procedures. [1] The main reason for surgery is painful knee osteoarthritis with reduced function. The second most common reason for a knee replacements is for inflammatory arthropathy. Total knee replacement has traditionally been offered to older people with intolerable knee pain, the loss of highly valued activities and severe end-stage knee osteoarthritis. [1] A knee replacement is an option for older adults who have severe knee pain and are not able to take part in the daily life activities and or physical activity that they enjoy. However, as you will learn from this blog this criteria has changed over time and there are some very important considerations not mentioned here that should be taken into account before making a final decision to undergo a knee replacement. Generally, people undergoing knee replacement have end-stage radiographic disease which is visible on an X-Ray. This means that a knee X-Ray shows “severe” knee osteoarthritis. Osteoarthritis is typically classified as mild, moderate or severe on X-ray. Here are some additional factors that need to be considered: [2]
Pathology (disease)
-Diagnosis of inflammatory arthritis or primary or secondary osteoarthritis. These two forms of osteoarhtritis have the same symptoms, but different causes; primary osteoarthritis has no known cause, while secondary osteoarthritis is caused by a pre-existing disease, injury, or joint misalignment.
-Radiographic changes - such as visible changes of the knee structure using X-ray imaging techniques.
-End-stage disease with exposed bone in at least one compartment of the knee. The knee is broken down into theree compartments on an X-Ray and when at least on of these compartments shows bone on bone it is classified as endstage osteoarthritis. You can see what this looks like in the X-Ray below.
Symptoms
-Severe knee pain during the day
-Severe night pain
-Substantial disability - for example, reduced walking distance and inability to work
-No improvement in pain or function with nonsurgical treatments such as pain medication, physical therapy, and regular rehabilitation exercises.
Patient
-Medically fit: they have no major medical issues that would result in a knee replacement causing medical complications
-Fully informed: the person understands the surgery including the risks and benefits and likely outcomes after surgery
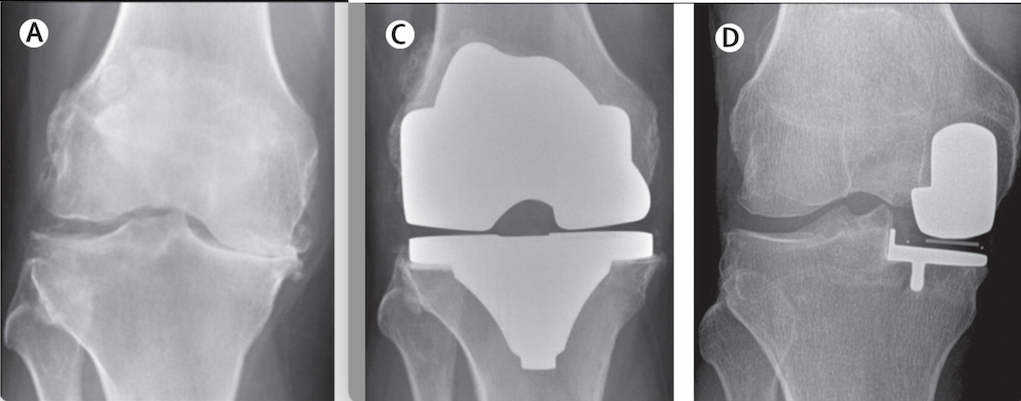
Image via Knee Replacement
Despite this criterion, the threshold for a knee replacement is not well defined and recent research has proposed to expand these traditional indications. The first contributor is placing more importance on your voice in decisions about whether to have a knee replacement. When you are engaged in conversations and decisions regarding a knee replacement, this is known as shared decision-making. [1] In a shared decision-making model, you have the ultimate say over whether to proceed with surgery or not, based on your own individual assessment of the risk versus benefit of having a knee replacement. There are many considerations for deciding if a knee replacement is the best option.
Assessments
Another patient-focused approach measures symptom burden to help with the decision-making process. This includes outcome assessments that include tests and instruments that provide valuable information. Self-reported patient outcome measures, that measure function, symptoms, and activity as well as assessments that focus on patient satisfaction can help you make your decision about surgery. A patient outcome measure is a simple questionnaire that is completed by the patient and it asks them about their pain and functional abilities as they relate to their knee pain. Each patient outcome measure provides you with a score that represents how much your knee pain is impacting your life. Here is one example of an patient outcome measure called the Knee Injury and Osteoarthritis Score (KOOS). In fact there is a free online tool that will allow you to obtain your KOOS score and compare it to others who also have knee pain and knee osteoarthritis. There are also functional performance tests, which includes the timed walk test, the up and go test, or the sit to stand test, which provide objective data to supplement the above mentioned outcome assessments. [2]
Physical Activity Importance
One research study is also questioning patients regarding a diverse range of physical activities and getting information about not only what they are able and unable to do, but also about what is important to them and the extent to which their participation was hindered by their knee disorder or pain. [3] It is important to note that when considering a knee replacement and not being able to engage in physical activity, there is evidence that a return to sports after a knee replacement is limited, and that the level of participation restriction increases when the demands of the sport increase. Although some people do return to sporting activities that they participated in before a knee replacement, there is an overall decrease in sports participation after surgery. [4] We’ve written a great blog about returning to sport after a knee replacement, specifically running after a knee replacement here.
Preoperative Status
It is also important to understand your preoperative status not only when deciding if a knee replacement is right for you, but also because your preoperative status is the strongest determinant of functional outcomes at six months and two years after a knee replacement surgery. [5] This means what you are able to do before your knee replacement will determine many of the things you can do after a knee replacement and also your limitations after a knee replacement. Preoperative pain and functional status were overwhelmingly the strongest determinants of outcomes at one year, and this remained true at two years after a knee replacement. The reality is that if you have more pain and your daily life is very limited before surgery you are more likely to have a worse outcome than people who have less pain and are more functional before surgery. Please discuss this with your surgeon so that you and your surgeon both understand your possible outcome after the surgery. Conversations like these help to manage people’s expectations after surgery. If a person has pain with taking the stairs and walking before surgery than it is unreasonable to expect to be able to jog after a knee replacement but it may be reasonable to be pain free with walking and using the stairs.
Another factor is a mental health score, as a low mental health score at the preoperative assessment is significantly associated with a lower outcome score at one year and two years after a knee replacement. [5] The findings from one study were obtained by administering the Short Form-36 (SF-36) patient questionnaire. The SF-36 is composed of eight multi-item scales (Physical Functioning, Role-Physical, Bodily Pain, General Health, Vitality, Social Functioning, Role-Emotional, Mental Health). There is a free online version of the Short Form-36 (SF-36) patient questionnaire if you would like a generic health-status measure. A range of psychological factors could be predictive of a poor outcome after surgery including depression, low self-efficacy, poor pain coping strategies and low social support. [4]
Conclusion
Although knee replacement surgery is one of the most commonly done and cost-effective musculoskeletal surgical procedures, there is more emphasis on the patient's voice in deciding whether or not to have a knee replacement. Although there is criteria for determining who should get a knee replacement, it is not well defined. This criteria should be considered, but you can also gain information from outcome assessment, self-reported outcome scores and functional performance tests. It is also valuable to look at what’s important to you and the extent to which your participation is hindered by your knee disorder or pain, your preoperative status and your mental health score. In a shared decision-making model, the patient has the ultimate say over whether to proceed with surgery or not, but that does not discredit your surgeon's advice. A shared-decision making model allows people and their surgeon to have an open discussion to make the best decision collaboratively.
Want to learn more about knee replacements? Try the Curovate app, an evidence-based app that will provide you with a physical therapy plan, guided video exercises and ways to measure and monitor your rehabilitation progress! Download Curovate today by clicking the links below.
 |
 |
|---|
Other recommended blogs
- Can I Kneel After a Knee Replacement?
- What is the Recovery Timeline for a Total Knee Replacement?
- How Can I Relieve Pain After my Total Knee Replacement?
References
1. Price, A. J., Alvand, A., Troelsen, A., Katz, J. N., Hooper, G., Gray, A., ... & Beard, D. (2018). Knee replacement. The Lancet, 392(10158), 1672-1682.
4. Wylde, V., Dieppe, P., Hewlett, S., & Learmonth, I. D. (2007). Total knee replacement: is it really an effective procedure for all?. The Knee, 14(6), 417-423.







