Osteoarthritis is a very common chronic condition in middle-aged and older adults and is currently the leading cause of disability worldwide. It is the most common form of arthritis. It affects the knees, hips, hands, neck, back, and big toes. It most commonly occurs in the knee and can involve more than one joint at a time.[1]
Osteoarthritis was thought of as “wear and tear” of the cartilage. We now know that this is not true, in fact, osteoarthritis affects the whole joint which includes the cartilage, bones surrounding the joint, as well as the joint fluid (synovial fluid) inside the joint. Osteoarthritis is a progressive disease of the whole joint in which the joint fails to repair the joint damage, which eventually leads to breakdown of cartilage, bone and a loss of healthy joint fluid.[2]
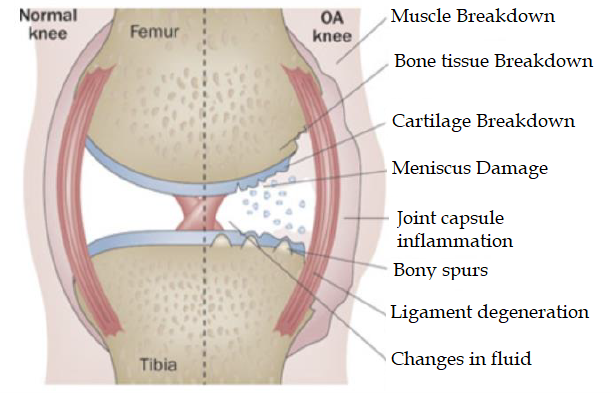
Image by Esther Waugh via Department of Physical Therapy, University of Toronto
You may be wondering, "If I have osteoarthritis, would I know it"?
Symptoms of osteoarthritis do not appear overnight, instead they build up over time and include:[3]
- Pain or aching in the joint during activity, after long periods of activity or at the end of the day.
- Swelling around the joint.
- Joint stiffness especially in the morning or after resting.
- Limited movement of the joint, also called limited range of movement.
- Muscle weakness around the joint.
- An unstable joint such as the knee feeling like it will give out on you.
Osteoarthritis affects a person beyond pain - it affects their sleeping patterns, energy level and mood which causes decreased activity levels and more pain! This vicious cycle can have a negative impact on your social, mental, and physical health. It may affect your mood, hobbies, relationships, and your job.[1]
It is challenging to target a single cause to prevent osteoarthritis. However, there are some known risks that are associated with osteoarthritis:[3]
- Age 50 and older – As we age, our bones, muscles and joints are also aging.
- Sex – Women are more likely to develop osteoarthritis than men. This is likely due to the fact that women have wider hips that are necessary for childbirth, but adds more stress on the knee joints in comparison to men. In addition, women experience menopause where the hormone levels necessary for joint health is lowered. These lower levels of hormones may also contribute to weight gain.
- Higher Body Mass Index (BMI) – BMI is a number calculated from a person’s weight and height. This number does go up as your weight goes up, and the extra weight puts more stress on the joints, therefore increasing risk of developing osteoarthritis.
- Obesity – Weighing more increases the stress on your joints. Having more fat cells in your body also contributes to osteoarthritis by producing chemicals that damage bones, cartilage, and all the joints in our body.
- Previous joint injury – There is a 50% increased risk of osteoarthritis for individuals who have had previous joint injuries such as damaging your cartilage or meniscus or any of the ligaments supporting your knee. Two common injuries to the knee are a tear of the anterior cruciate ligament (ACL) and a meniscus tear. However, if you have had a previous joint injury, osteoarthritis is preventable with diet, exercise and lifestyle!
- Genetics - Irregular joint and bone shape at birth can cause stress to joints over time. A common example is the hip. The hip is made of a ball and socket joint. In a healthy human, the ball and the socket fit perfectly together. In some cases, the ball and socket does not fit perfectly, causing stresses to some parts in the joint. Over time, this pressure on the joint can cause osteoarthritis.
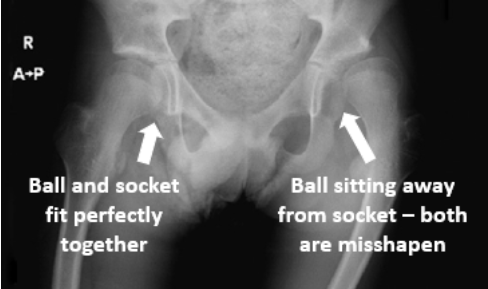
Image by Donald Neumann via Kinesiology of the Musculoskeletal System
If you suspect you have osteoarthritis, please see a healthcare professional to receive guidance for your exercises, diet and necessary lifestyle modifications.
Management/Treatment for Osteoarthritis
Going with the common saying “prevention is better than a cure”, some risk factors are modifiable such as BMI and obesity. On top of that, although osteoarthritis is more likely to affect a person older than 50 years old, it is not a natural and inevitable part of aging, as it can be prevented with self-management such as exercise, diet, and a healthy lifestyle.[3]
The treatment and management of osteoarthritis can be visualized as a pyramid:
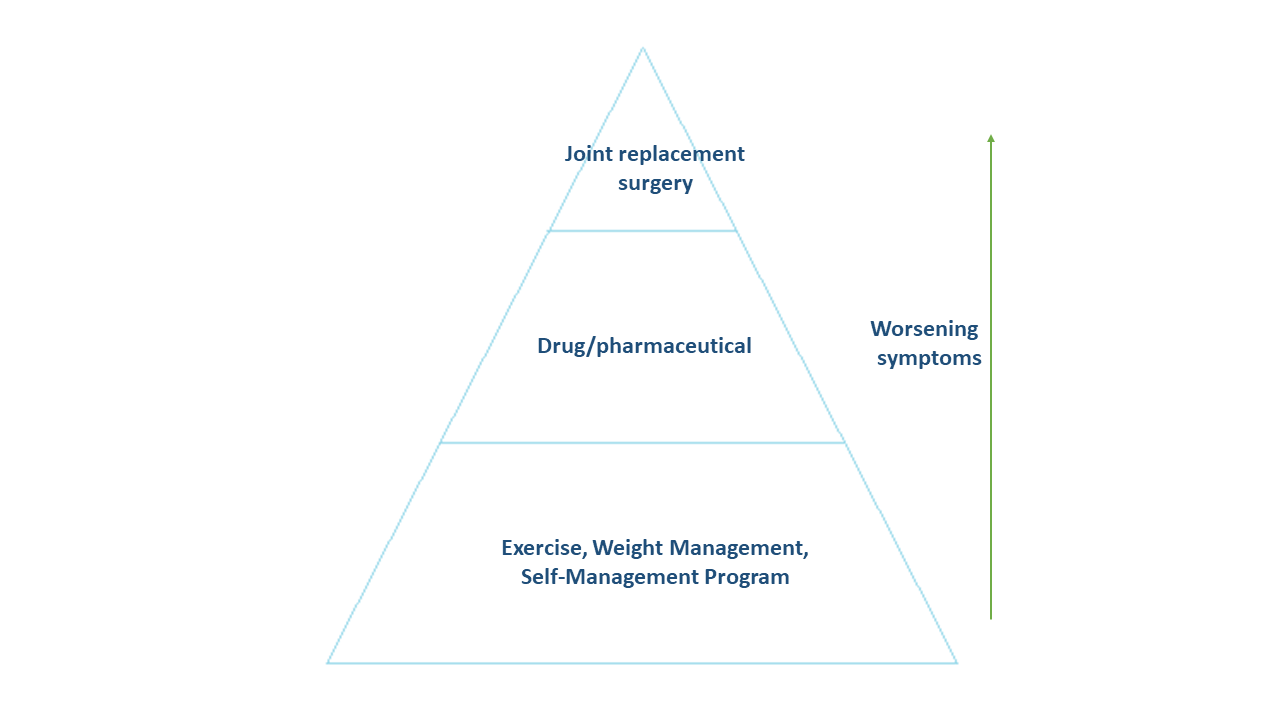
When a person is diagnosed with osteoarthritis in the early stages, the healthcare team or physical therapist will prescribe therapeutic exercises, weight management and self-management programs. As the disease progresses, licensed professionals may prescribe some drug therapy in addition to the exercises and management programs. If the symptoms continue to worsen, you may need to go through a joint replacement surgery, such as a total knee replacement, you can read more about it here.[2]
If you are scheduled for a total joint replacement surgery, it is recommended that you start your pre-habilitation as soon as possible for a better surgical outcome! Wondering what pre-habilitation is? Read more about it here! Following surgery, you will also begin your rehabilitation immediately.
Curovate is a physical therapy app that has a built in recovery plan for knee and hip replacement surgeries. This plan tracks your recovery journey by using video guided exercises, reminders, and the ability to measure the movement of your joint (called range of motion). Your exercises will gradually get harder as you begin to regain your movement and strength, helping you to recover over time. To try the app today, click the download links below.
If you need further customized assistance during your surgery or injury recovery check out our Virtual Physical Therapy page to book your 1-on-1 virtual physical therapy sessions with a physical therapist.









